Redefining Parkinson's to match how Patients feel, not what others see!
Parkinson's patients know their disease better than anyone, their description of PD is the right one.
My wish for everyone affected by Parkinson’s in 2025, is to change the definition of Parkinson’s from that which Neurologists observe from the outside to that which Patients feel from the inside.
All Parkinson's Patients remember the day that they were diagnosed with Parkinson's disease. You may have noticed growing stiffness in your arms and legs, You often had periods of intense fatigue or brain fog that you couldn't explain and odd pains in your legs and feet. You may have been suffering from constipation for years, or more recently, from urinary urgency ... but that almost insignificant tremor in one hand was niggeling. Your general practitioner suggested that you see a specialist, in this case a neurologist.
The misdiagnosis of Parkinson’s disease.
On this first visit, your Neurologist may have asked you to do a certain number of movement exercises: sitting down, standing up, rotating your hands and tapping your feet, walking, touching your nose with one finger, taking the pull-back test... and then the diagnosis was announced: "You have Parkinson's disease!"
One question that your Neurologist didn't ask you was: "How do you feel, what symptoms do you have, how long have you had them?"
You were not asked that question, because the purpose of the visit was not to discuss the full range of symptoms that had led you to make the appontment. You were not invited to open your "Pandora's Box" of various maledictions that have been wreaking havoc with your life for the past decade. No, this was a technical visit designed to answer just one question: "Do you have the visible “motor” symptoms consistent with the movement disorder that neurologists call Parkinson's disease?"
Once that question had been answered, patients are “classified” as suffering from Parkinson's disease, where the disease is defined purely in terms of a limited neurological model. Unfortunately, that limited model of Parkinson’s disease doesn’t actually exist by itself. The Parkinson’s that people actually actually suffer from is a syndrome, involving disorders in many other organs throughout the body which give rise to a much wider range of symptoms as well as the aforementioned neurological condition. The combination of using only a limited set of symptoms to confirm a theoretically simplified disease medel there fore leads to a misdiagnosis.
The consequences of misdiagnosis
Patients are misdiagnosed because they are not asked about the diverse range of “non-motor” symptoms that they suffered from for years before the motor symptoms appeared, which are the hallmark of Parkinson’s syndrome. This misdiagnosis has grave consequences for the patient. Patient care is transferred entirely to neurologists whose expertise and scope for examination and care is limited to the neurological aspects of the disease. The non-neurological components of Parkinson’s syndrome become orphan conditions of Parkinson’s, misunderstood, disregared and untreated. Medical examination and care therefore fall far short of that expected for the disease that patients actually suffer from. Patients have no way to resolve this absence of care, because Parkinson’s syndrome is not recognised. Almost all Parkinson's patients are locked into the consequences of that visit for the rest of their lives.
My Parkinson's wish for 2025, is to change the definition of Parkinson’s from that which Neurologists see from the outside to that which Patients feel from the inside.
You may not consider this objective to be very ambitious, after all it is just common sense. Let me make it clear, such a change would be revolutionary. If adopted, it would lead to a radical improvement in how patients are cared for and open up new avanues for research. The idea is simple and the potential benefits for patients would be considerable, but making it happen will not be easy. This idea can be summed up in the following statement:
The current neurological definition of Parkinson's disease is incomplete and misleading. It doesn't match the severity and diversity of the lived-experience of Patients, which in turn leads to misdiagnosis and inadequate patient care.
This idea builds on the message, delivered by Dr Laurie Mischley in her recent video presentation on Parkinson's information platform No Silver Bullet 4 PD. In that presentation Dr Mischley made a passionate plea for "Rebranding Parkinson's", because the way Parkinson's disease is currently defined is failing patients in many ways. Patients are not getting the best care and research is not delivering any tangible improvements regarding new therapies.
What is the current definition of Parkinson's and why is it wrong?
Parkinson's disease is currently defined as a neurological disorder, a disease of the brain that controls movement which is deemed to begin with the occurrence of motor symptoms. Because of this definition, patients are assigned to neurologists for diagnosis and thereafter for care. To diagnose Parkinson's, neurologists check for the presence of the cardinal "motor symptoms" of Parkinson's; rigidity, slowness of movement, postural stoop, small steps, cogwheel joint movements, tremor. Their presence confirms the exsitence of Parkinson's disease.
Based on the match between the definition of the disease and the symptoms considered, the diagnosis is technically correct. But because the definition of Parkinson's does not match the reality of the disease, it leads to misdiagnosis.
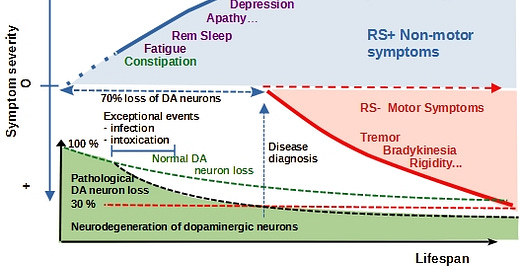
Fig 1) The current neurological model for Parkinson’s. Parkinson’s disease is limited to the brain and the period following the loss of up to 70% of dopaminergic neurons. All events ocurring before the appearance of motor symptoms and non-motor symptoms are not considered to be integral parts of Parkinson’s disease.
The consequences of this incomplete definition are devastating
From this point on, patients are assigned to neurologists for care, but the latter have very little to offer them. Neurologists tell their patients that there is no cure for Parkinson's and no approved therapies to slow or stop its progression. The basic care is largely limited to medication to attenuate the motor symptoms of Parkinson's disease. To quote Dr Laurie Mischley:
“The current system of care for Parkinson’s is purely palliative.
We try to improve your comfort as you go downhill.
That’s what I’m here to change.”
Dr Laurie Mischley
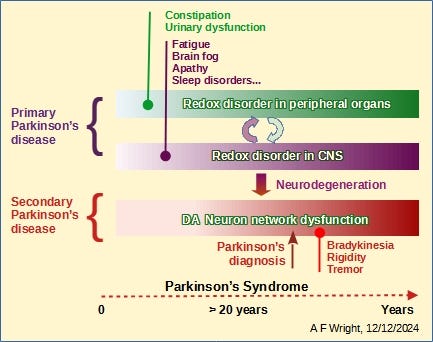
The diagnosis is incomplete because Parkinson's is not a single disease. It is the manifestation of two (or more) diseases running in parallel. Apart from the neurological disorder, Parkinson's Patients are also suffering from a chronic, metabolic disease that started over the 20 years prior to diagnosis and caused the loss of up to 70% of neurons which make dopamine at the time of diagnosis. Beyond that, both diseases continue in parallel, but no medical specialists are assigned to look into the non-neurological aspects of Parkinson’s. Neurologists do what they can to treat the neurological aspects of Parkinson's with the limited means at their disposal. This is a "Catch 22" situation. There is no-one else to turn to.
Patients are locked into a system that condemns them to programmed decline without any care or support for the chronic condition that drives the progression of the disease.
How can we change this situation?
A potential solution lies in changing the definition of Parkinson's to include the long period prior to diagnosis during which a large proportion of dopamine neurons are lost and taking into account all the symptoms present over the whole duration of the disease including those originating in peripheral organs well before motor symptoms appear. This change could lead to a radical improvement in how patients are cared for and how research is conducted.
The current definition of Parkinson’s disease covers the period that begins late in the disease, after the appearance of motor symptoms (a marker of severe neurological disorder) and terminates with the death of the patient. It only takes into account motor symptoms and the late-stage neurological aspects of the disease. This definition has failed to deliver tangible benefits for Parkinson’s patients for the last 4 decades. However it will only be declared obsolete and abandoned if we can replace it with a better one.
Changing hearts, minds and practices across the whole Parkinson's community will take considerable time and effort. It can only happen if a determined and influential group of people embraces and promotes a new definition for Parkinson’s that will render the current model obsolete. That group will include Parkinson’s patient advocates, researchers, scientists and medical professionals. I invite you to raise your hand and become part of an action group with the objective to: Change Parkinson’s 2025 .
Change Parkinson’s 2025 – a call to change the definition of Parkinson's
Change Parkinson’s 2025 should embrace a much more realistic description of Parkinson’s than the model currently in use. By starting up to 2 decades before Parkinson’s is currently diagnosed and embracing all the symptoms; including those that are markers of reversible, non-neurological pathologies, Change Parkinson’s 2025 doesn’t have to terminate with the death of the patient. On the contrary it opens the door to following and treating the disease well before the advanced neurological disorder takes hold. This also means encourageing medical professionals other than neurologists to take an interest in the treatment of Parkinson's well before neurological symptoms appear. In practice, this could include dietary recommendations, blood and urine tests to track metabolic disorder, oxidative stress and imflammation as proposed by Dr Laurie Mischley. Parkinson's will not be resolved by neurologists. It can only be resolved by closely following Parkinson's patients and studying the earlier stages of the disease, well before motor symptoms appear.
What is the nature of the disease responsible for the loss of dopamine neurons ?
Leading researchers hold the view that the unidentified disease responsible for the loss of dopamine neurons is a combination of oxidative stress and mitochondrial dysfunction. This view guided my own research to reduce oxidative stress in peripheral organs and neurons by activating the Nrf2 transcription factor using sulforaphane. I have used this technique with good results to control my own Parkinson’s, but other conditions are very likely contribute to this neuron loss. The objective is to replace the restricted, late stage, motor-symptom, brain-centric model by one that includes all the symptoms, systems and chronology, closely matching the reality that Parkinson’s patients live with on a daily basis.
Fig 2) Parkinson’s is 2 diseases which develop in a specific order, then progress in parallel. Primary Parkinson’s disease is a reversible metabolic disorder which damages cells in peripheral organs and neurons in the CNS. Because damaged neurons are not replaced by new ones, neuron damage and loss creates widespread structural neuronal network disorder that is manifested as Secondary Parkinson’s disease in the CNS.
Fig 3) Parkinson’s Syndrome is a multi-system syndrome resulting from the simultaneous expression of both Primary and Secondary Parkinson’s. The existence of Primary Parkinson’s is ignored by the whole medical profession.
Fig 4) Parkinson’s Syndrome (PS) is characterized by its full range of symptoms over the whole period of the disease, including those occurring many years prior to the current point of diagnosis. By ignoring the early stages and failing to take non-motor symptoms into account, the neurological aspects of PS take hold with disastrous consequences. Imagine the changes in care and prevention that would follow the adoption of this comprehensive model for Parkinson’s syndrome.
Responding to this initiative
If you believe in the utility of this initiative and wish to support this action or play an active role in any future organisation, please leave a comment indicating how you might contribute.
The articles and information that I will be sharing with you are the result of more than 10,000 hours of hard work and experimentation extending over more than 5 years. My initial objective was to try to understand Parkinson’s enough to treat my own disease and share the results with other Parkinson’s patients. That objective was achieved in 2022. The present objective is to improve how Parkinson’s is cared for and treated for the benefit of all Parkinson’s patients. That is a much more difficult task, but deserves to be given a try. Please give some thought to this when you click on the subscribe button.







Not sure what I can do but I share your info with my local support group.
I totally agree with yourself and Dr Mischley. I am reversing my PD using many things and I am confident I will get even better. I am trying DMSO and MSM and struggle with the smell lol which stops me taking higher, consistent doses but I have hope smaller doses long term will work.
I have tried drinking broccoli tea but found the process difficult. My latest novel experiments are hbot, lithium, ginkgo, dmso, MSM, and about to start nicotinamide riboside. I'd like to try an NAD IV drip but the cost is prohibitive.
Something that has also provided great relief is low dose naltrexone which helps immensely. I've read it works on toll4 and ogfr pathways which may slow progression they think. I wish this info was more well known to people.
I was just diagnosed with early onset PD by the exact physical exam you described. I’d like to learn everything I can to stop my symptoms from progressing. Thank you.